Parameatal Urethral Cyst in Adult: Should be Excised
Article information
Abstract
The formation of cysts in the parameatal area has been reported as rare. A parameatal urethral cyst is a congenital anomaly and has been reported even more rarely in adults. In this study, we present two cases of parameatal urethral cyst and aim to investigate their causes and treatment methods. The extent of cyst spread was assessed using a urethroscope prior to cyst excision, and the excision range was determined accordingly. Complete excision of the cyst was performed as the treatment for parameatal urethral cyst. Both patients were adults who presented with urinary symptoms related to the cyst, necessitating the excision of the congenital parameatal urethral cyst.
Introduction
Cyst formation in the parameatal area was first reported in two male cases in 1956. The disease is extremely rare, with only approximately 40 cases reported worldwide since then [1]. Although parameatal urethral cyst is associated with various medical specialties such as urology, dermatology, pediatrics, and plastic surgery, it is often considered unfamiliar, and treatment methods for it are diverse [2]. Here, we report two cases of cysts in the parameatal area in adults. We aimed to investigate the causes and treatment methods for these cases.
Case report
In the first case, an 18-year-old male who had undergone circumcision presented to our clinic with a cyst in the penile glans. He had been aware of the cyst for the past ten years and experienced lower urinary tract symptoms (LUTS). He had previously sought treatment at other hospitals, where aspiration was performed initially but the cyst recurred. Subsequently, observation was suggested at a second hospital. During the physical examination, a painless single mass measuring 8 x 9 mm in size, with a spherical and soft cystic form, was found on the left side of the urethral meatus of the penile glans (Fig. 1). For the treatment, the extent of cyst spread was initially inspected using a cystourethroscope under spinal anesthesia. Subsequently, the cyst was enucleated and completely removed. Cyst bed coagulation and anastomosis were performed to prevent recurrence. During the one-year follow-up period, there were no instances of stricture in the urethral meatus, cosmetic issues, or LUTS.

Preoperative parameatal urethral cyst. (A) 18-years-old man with cystic lesion of left parameatus. (B) 8 x 9 mm sized cyst was located on the urethral meatus close to the inner margin of the orifice.
In the second case, a 31-year-old male who had undergone circumcision visited our clinic with a cystic formation around the urethral meatus and related symptoms. He had been aware of the cystic formation for the past fifteen years. After getting married, he complained of intermittent terminal dribbling, a feeling of irritation, and discomfort during intercourse. A cystic mass measuring approximately 1 cm in size was identified on the left side of the penile glans. The treatment approach for this case was the same as that of the first patient. A urethral catheter was inserted and remained in place for 3 days. During the one-year follow-up period, there was no recurrence of the cyst, and the patient did not report any problems with voiding or discomfort during intercourse.
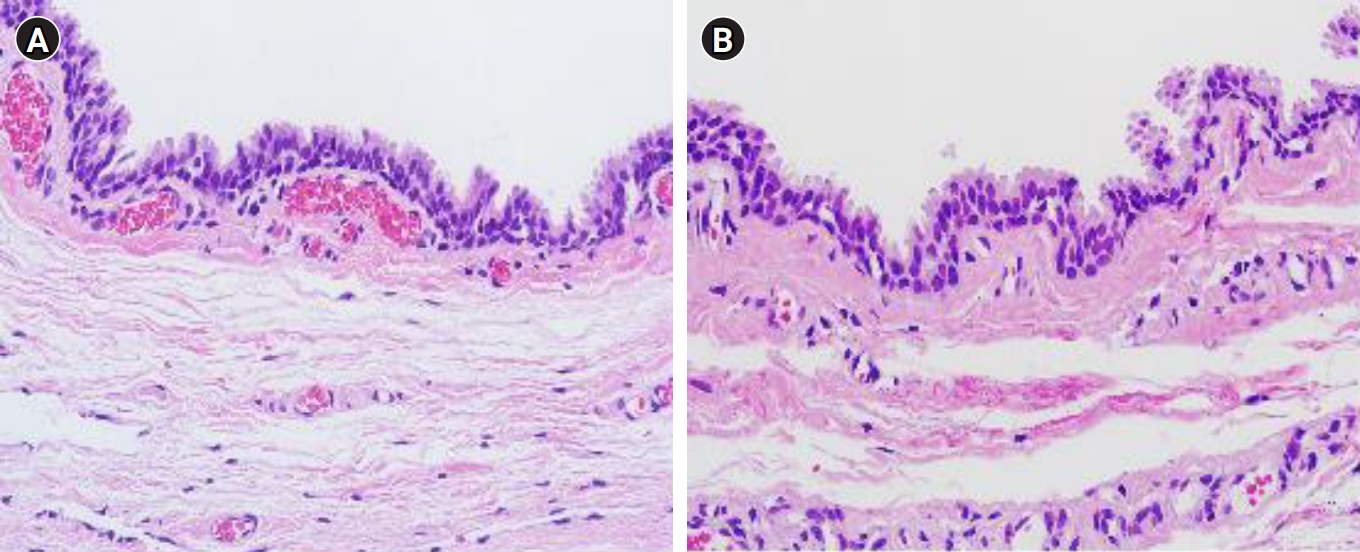
The pathological characteristics of the tissues in the two cases were similar. The cysts exhibited a laminar surface wall composed of ciliated and non-ciliated pseudostriated columnar epithelium (Fig. 2). The cystic fluid was mucinous in nature, and no inflammatory cells were observed within it.
Discussion
Since its first report by Thompson and Latin [1] in 1956, parameatal urethral cyst has been recognized to occur in males, including infants, children, adults, and even females [3]. It was previously referred to as a mucoid cyst or apocrine cystadenoma, and additional clinical diagnoses such as dysembryoplastic cyst have been added [4]. Parameatal urethral cysts are typically smaller than 1 cm in size and are often discovered incidentally. They are commonly located on the lateral margin of the urethral meatus, with bilateral occurrences being rare [2]. Although most cases are asymptomatic, some may present with urinary retention, dysuria, painful sexual intercourse, poor genital cosmetic appearance, or alterations in urinary stream distribution, requiring treatment. In our cases, active treatment was pursued due to discomfort during sexual intercourse and poor genital cosmetic appearance. Otsuka et al [2] classified parameatal cysts into three types based on histopathological characteristics. The first type is the urethral type cyst, composed of stratified columnar, cuboidal, and/or transitional epithelium, accounting for the highest proportion at 70.1%. The second type is the epidermal type cyst, composed of squamous epithelium, accounting for 10.9%. The last type is the mixed type cyst, which is composed of columnar, transitional, and squamous epithelium, accounting for 4.6% [2].
Regarding this classification, Neeli et al [5] reported that parameatal urethral cysts were classified based on the segment origin of the cyst within the urethra. In our study, we determined that our two cases, characterized by pseudostriated columnar epithelium, belonged to the urethral cyst type.
The etiology of parameatal urethral cysts is not clearly understood, and various hypotheses regarding the embryogenesis of the cysts have been proposed. Thompson and Lantin [1] demonstrated, through the transection of embryonic glans penis at 7.5 and 8 months, that the cysts develop from the continuous presence of a cystic space along the separation line of the prepuce of the penile glans. Shiraki [6] suggested that a congenital anomaly in the embryogenesis of the paraurethral duct occurs due to secondary triggers such as infection or injury. The paraurethral duct is divided into an internal duct and an external duct. The internal duct is associated with the origin of hypospadias, while the external duct is involved in the differentiation of the frenulum and meatus through the median raphe of the frenulum, scrotum, and penis [6]. Additionally, Hill and Handley [7] proposed that infection could be a cause of obstruction. However, Otsuka [2] demonstrated that the cyst formation described by Thompson and Lantin [1] corresponds to an epidermal cyst, histologically composed of epidermal components, rather than a urethral type cyst.
The treatment of parameatal urethral cysts should focus on cyst removal, prevention of recurrence, and achieving satisfactory cosmetic results. It is important to ensure that there are no voiding problems or discomfort during sexual intercourse after treatment. Various treatment methods have been reported for parameatal urethral cysts, including surgical excision, waiting for spontaneous rupture, needle aspiration, and marsupialization of the cyst [5]. In children, spontaneous rupture of the cyst is rare, and there is a risk of infection, inflammation, and bleeding. The effectiveness of conservative treatment is not well established. Aspiration of the cyst contents carries a high risk of recurrence, as evidenced by the recurrence observed in one of our cases. Marsupialization of the parameatal urethral cyst may result in unsatisfactory cosmetic outcomes and can also be associated with a risk of recurrence due to the presence of residual cyst remnants [8].
Accordingly, complete excision of the cyst is considered the treatment of choice for parameatal cysts. It is crucial to completely and sharply excise the cyst wall, remove any cavity extensions, and ensure that no cyst remnants are left behind, as emphasized by Wills et al [9].
In our cases, we utilized cystourethroscopy to assess the extent of cyst spread before performing the cyst excision. This step was essential in determining the appropriate extent of excision, with the aim of preventing cosmetic issues and post-treatment discomfort during urination. This procedure plays a significant role in achieving optimal outcomes.
Notes
Conflict of interest
The authors declare no conflicts-of-interest related to this article.