Long COVID Syndrome: Clinical Presentation, Pathophysiology, Management
Article information
Abstract
Long coronavirus disease (COVID) syndrome is persistent symptoms and complications that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 infections. Symptoms associated with long COVID can vary widely from person to person but commonly include: fatigue, shortness of breath, chest pain or discomfort, joint pain, difficulty concentrating (brain fog), headache, loss of taste or smell, sleep disturbances, palpitations, persistent cough. Possible pathophysiologic theories are viral persistence, dysregulated immune response, autoimmune response, endothelial dysfunction, gut dysbiosis, damage to organs and tissues, neurological involvement, post-viral syndrome. Although current diagnostic and treatment options are insufficient, the management aim to alleviate symptoms, improve quality of life, and support recovery. The possible therapies and interventions that may be considered are symptomatic management, rehabilitation and exercise, respiratory support, cognitive and psychological support, sleep management, nutritional support, support groups and patient education, anti-inflammatory drugs, immuno-modulatory therapies. For patients enduring prolonged suffering from this long COVID syndrome, a multidisciplinary approach is essential for comprehensive management.
Introduction
Long coronavirus disease (COVID) syndrome, also known as post-acute sequelae of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, refers to a condition in which individuals experience persistent symptoms and complications following the acute phase of a COVID-19 infection. Long COVID syndrome can affect individuals of all ages, including those who had mild or moderate initial COVID-19 symptoms [1].
About 10% (65 million) of COVID-19 infected people around the world have long COVID syndrome. The incidence is estimated at 10–30% of non-hospitalized cases [2], 50–70% of hospitalized cases [3], and 10–12% of vaccinated cases [4]. Long COVID is associated with the highest percentage of diagnoses between the ages of 36–50 years, and most long COVID cases are in non-hospitalized patients with a mild acute illness [5].
Clinical Presentation
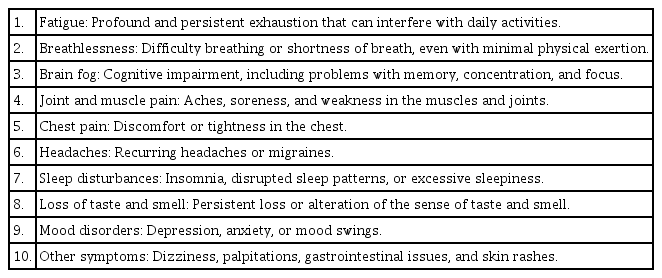
The defining characteristic of long COVID syndrome is the persistence of symptoms for weeks or months after the acute phase of the illness has resolved. Symptoms associated with long COVID can vary widely from person to person but commonly include: fatigue, shortness of breath, chest pain or discomfort, joint pain, difficulty concentrating (brain fog), headache, loss of taste or smell, sleep disturbances, palpitations, persistent cough (Table 1).
The World Health Organization (WHO) defines a symptom that occurs within three months of COVID-19 confirmation and lasts more than two months as "long COVID-19." The most common symptoms are fatigue, decreased vitality, and shortness of breath [6]. In Korea, a research team of Seoul National University Hospital followed 147 patients confirmed with COVID-19 for more than three months and 55.8% of them complained of long COVID-19 symptoms. The most common persistent symptoms were chronic fatigue (32.7%), memory loss (15%), olfactory disorders (14.3%), anxiety (9.5), myalgia (7.5%), hypogeusia (6.8%), and dizziness (6.8%) [7].
Long COVID-19 increases adverse outcomes, with new-onset cardiovascular, thrombotic and cerebrovascular diseases, type 2 diabetes, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), dysautonomia, and postural orthostatic tachycardia syndrome (POTS). These symptoms can last for years, and new-onset ME/CFS and dysautonomia are expected to be lifelong.
Pathophysiology
The exact cause and pathophysiology of the persistent symptoms are not fully understood, and many studies are still in progress. Possible pathophysiologic theories are viral persistence [8], dysregulated immune response [9], autoimmune response [10], endothelial dysfunction [11,12], gut dysbiosis [13], damage to organs and tissues [14], neurological involvement [15], post-viral syndrome [16,17] (Table 2).
Multiple studies have revealed multi-organ damage associated with COVID-19. In a 1-year follow-up study with 536 participants, examining the heart, lungs, liver, kidneys, pancreas and spleen, found that 59% had single-organ damage and 27% multi-organ damage.
Risk factors potentially include female sex, type 2 diabetes, Ebstein-Barr virus reactivation, the presence of specific auto-antibodies, connective tissue disorders, attention deficit hyperactivity disorder, chronic urticaria, allergic rhinitis, Hispanic or Latino heritage, lower income and an inability to adequately rest in the early weeks after developing COVID-19 [18].
It's important to note that these theories are not mutually exclusive, and it's likely that multiple factors contribute to the development of long COVID syndrome. Ongoing research is focused on understanding the underlying mechanisms and developing effective treatments for this condition.
Management
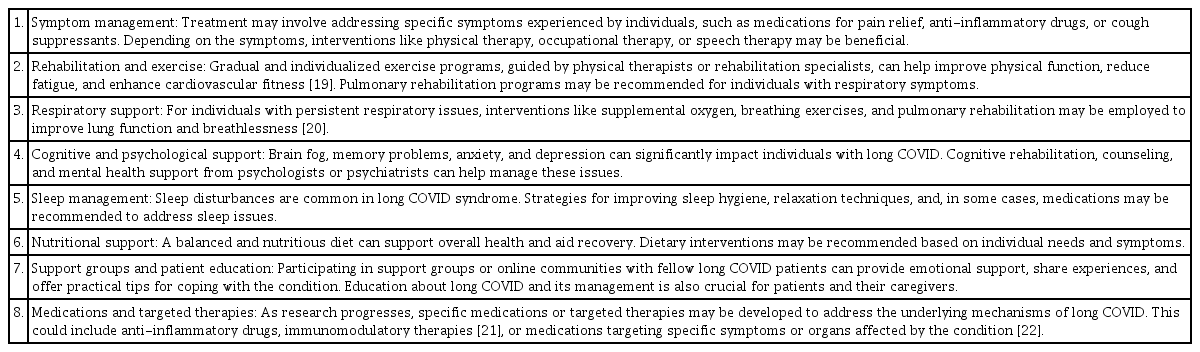
Although there are no broadly effective treatments of long COVID syndrome, the management and treatment aim to alleviate symptoms, improve quality of life, and support recovery. Since long COVID syndrome encompasses a wide range of symptoms and affects individuals differently, a multidisciplinary approach involving various healthcare professionals may be necessary. The possible therapies and interventions that may be considered are symptomatic management, rehabilitation and exercise, respiratory support, cognitive and psychological support, sleep management, nutritional support, support groups and patient education, anti-inflammatory drugs, immuno-modulatory therapies (Table 3).
Many strategies for ME/CFS are effective for individuals with long COVID, including pacing and symptom-specific β-blockers for POTS, low-dose naltrexone for neuroinflammation and intravenous immunoglobulin for immune dysfunction) and non-pharmacological options (salt intake, cognitive pacing, and elimination diets for gastrointestinal symptoms).
The treatment for long COVID syndrome focuses on managing the individual's symptoms and improving their quality of life. This may include a multidisciplinary approach involving healthcare professionals such as primary care physicians, specialists, physical therapists, occupational therapists, mental health professionals, and rehabilitation specialists.
It's important to note that the treatment approach for long COVID syndrome is highly individualized, and healthcare professionals will assess and tailor interventions to each person's specific needs and symptoms.
Official health websites for the latest developments in the understanding and management of long COVID syndrome are: World Health Organization (https://www.who.int/), Centers for Disease Control and Prevention (https://www.cdc.gov/coronavirus/2019-ncov/index.html), National Institutes of Health (https://www.nih.gov/), European Centre for Disease Prevention and Control (https://www.ecdc.europa.eu/), The Lancet and Journal of the American Medical Association (JAMA).
Conclusion
Long COVID syndrome is a condition where individuals continue to manifest a variety of symptoms even after confirming a COVID-19 infection. Patients often experience prolonged difficulty in coping with the aftermath. While various mechanisms and risk factors have been suggested, there is still a lack of definitive evidence in certain areas. However, for patients enduring prolonged suffering from this long COVID syndrome, a multidisciplinary approach is essential for comprehensive management.
Notes
Conflict of interest
The authors declare no conflicts-of-interest related to this article.