Study on the Learning Environment of Medical Students in the COVID-19
Article information
Abstract
In Korea, the COVID-19 pandemic began and the situation was very serious due to the rapid increase in confirmed cases. In this study, we conducted a study that included the online class environment, learning environment including living environment, and overall life of medical students who are experiencing sudden changes in environment due to COVID-19, to help medical students' academic and school life, and to provide medical services. We want to help improve the quality of education. The subjects of the study are 6 grades from the 1st year of pre-medical school to the 4th year of the medical department attending a medical school in the Daegu area in the 2021 school year, and a total of 450 are studied. In addition, a survey was conducted on students who agreed to the study, and it consisted about the online learning environment and overall living conditions. As a result of the study, there were no gender differences in the online learning environment and overall life amid the COVID-19 pandemic. There were differences between pre-medical and medical students in the online learning environment, and overall life. Due to the sudden COVID-19 pandemic, medical students were faced with an online learning environment that they could not choose. They took care of the physical resources provided by the school on their own and learned the importance of this.
Introduction
‘COVID-19’, which broke out in 2020, is evaluated as one the most powerful pandemics [1]. The outbreak of COVID-19 changed the lives of many people around the world, including the economy, society, and culture, and among these, communication methods are evaluated as the area that has changed the most rapidly. It has been reported that communication that previously took place face-to-face is now being done non-face-to-face in almost all areas, and in particular, non-face-to-face communication methods have appeared the fastest in school education [2,3].
In the case of Korea, the COVID-19 situation was very serious as it was recognized globally as a risky country due to the rapid increase in confirmed cases at the beginning of the COVID-19 outbreak, and was designated as a country with entry restrictions by almost all countries. Accordingly, all schools switched to entirely non-face-to-face online classes, and online schooling and online-centered school classes were unprepared and had to go through a lot of trial and error, causing many problems [4,5].
Korean schools quickly switched to online classes despite the sudden change, and through much research on online classes and efforts to find improvements, student and instructor satisfaction with online classes increased [5,6]. After COVID-19, research and interest in school education have focused on online classes, including real-time interactive classes and content utilization, but classes only represent a part of the education that schools are responsible for.
The ultimate premise and purpose of school education is equality of educational opportunity and equality of educational results. In particular, equality of educational outcomes is the goal of a developed society and one of the most important goals of education [7,8]. Therefore, schools must provide students with an environment where everyone can learn equally. However, in the COVID-19 situation, schools only provided online classes and failed to provide all environments in which to receive classes, and it was reported that online-centered school education in the COVID-19 situation further strengthened the learning gap among students [9,10]. In particular, the learning gap among students was large depending on family circumstances [9]. In addition, students' difficulties were found not only in online classes, but also in many other areas, such as poor academic performance, life management and learning management, friendship and family relationships, and emotional problems [10,11].
In particular, it has been reported that medical students experience a lot of stress even before the COVID-19 pandemic [12]. In addition, it was found that the COVID-19 situation also adds stress to medical students, which is related to learning and acts as a hindrance to medical school education [13]. In Korea, medical students have a significant degree of learning about medical specialties, and almost all education is conducted face-to-face (offline) [14]. It can be seen that the COVID-19 pandemic has a significant impact on the learning of medical students, and that not only medical students' classes, but also the overall learning environment, including emotional issues, human relationships, and life, are all important. However, no research has been reported on the learning environment needed for medical students due to the COVID-19 pandemic.
Against this background, in this study, we conducted a study that included the online class environment, learning environment including living environment, and overall life of medical students who are experiencing sudden environmental changes due to COVID-19 to help medical students with their studies and school life. And we also aim to help improve the quality of medical education. Therefore, this study set the following research questions.
First, we want to learn about the online learning environment amid the COVID-19 pandemic and verify whether there are differences according to gender and medical school course. Second, we would like to learn about the overall life of medical students in online-centered school life amid the COVID-19 pandemic and conduct research on differences according to gender and medical school courses.
Methods
1. Subject of study and data collection
The subjects of the study are 6 grades from the 1st year of pre-medical school to the 4th year of the medical department attending a medical school in the Daegu area in the 2021 school year, and a total of 450 are studied. The survey was conducted from August 1st to August 30th, when the first semester of the 2021 school year ended, it was administered to the research subjects, including a recruitment notice and consent form for research participants. The recruitment notice explained the research purpose, research method, and study content in detail, and sent an address to an online survey site containing a consent form, asking participants to fill out an online consent form and survey. The survey was designed so that if the research subject did not consent, the survey could be stopped immediately.
2. Instruments
The research tools are a questionnaire developed previously and implemented to suit the context of the medical school being studied, and a tool developed by the Research Information Center of the Seoul Metropolitan Office of Education [15]. Additionally, we developed additional survey questions suitable for investigating the overall learning environment of medical students. Three medical education experts and two education experts with more than 10 years of medical school education experience participated in the development of the questionnaire. The survey consists of questions about medical students' online learning environment and living conditions amid the COVID-19 pandemic.
3. Statistical analysis
The collected data were analyzed using IBM SPSS ver. 27.0 (IBM Corp., Armonk, NY, USA) as follows. A chi-square test was conducted to verify differences in the online learning environment in the COVID-19 pandemic situation, differences in living conditions in the COVID-19 pandemic situation between pre-medical and medical students, and gender. A t-test was conducted to verify the difference in sleep time during the COVID-19 pandemic.
4. Ethical statements:
For research ethics, a notice and consent form with sufficient explanation were provided prior to the survey, and an online survey was designed so that only students who voluntarily agreed to participate could respond. Even during the survey, if respondents did not want to take the survey, they could stop immediately, and this was announced in advance.
Results
1. Characteristics of participants
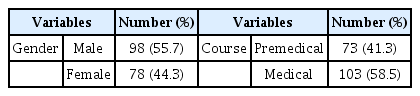
Of the 450 students who responded 39.1% (176), including 73 (41.3%) of the pre-medical and 103 (58.5%) of the medical students. Regarding gender distribution, 98 (55.7%) of male students and 78 (44.3%) of female students responded (Table 1).
2. Differences in online learning environments in the COVID-19 pandemic
1) The best part
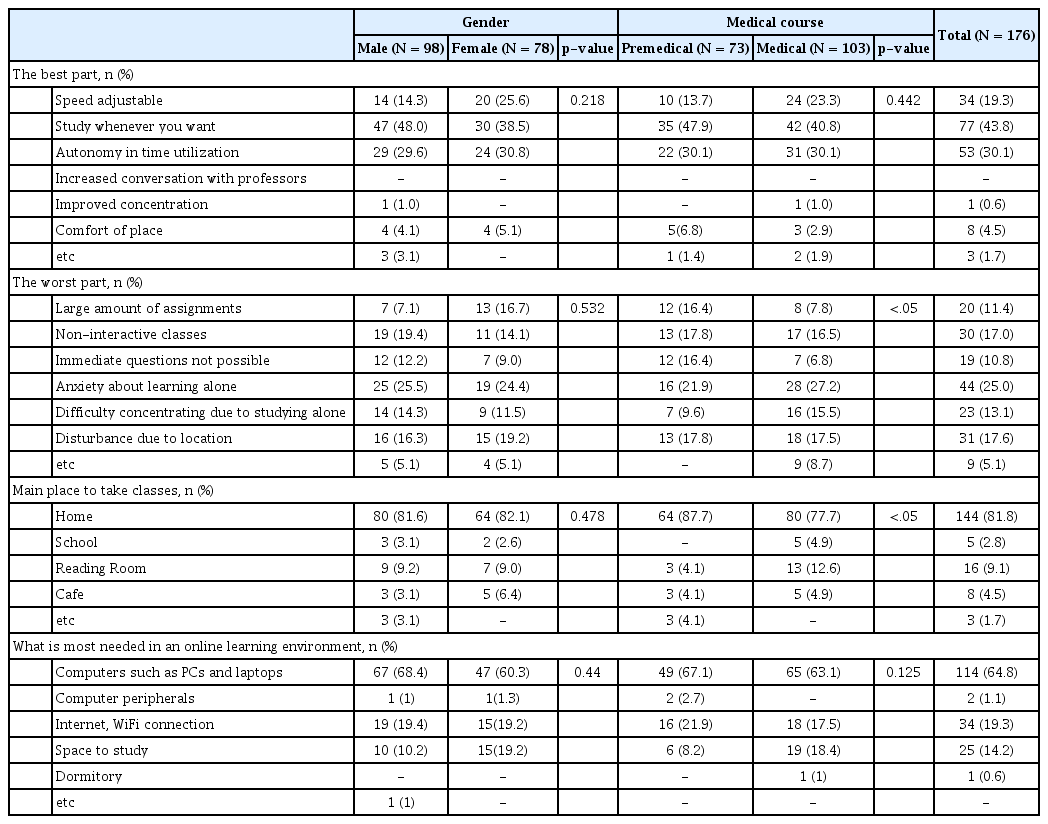
The best part about the online learning environment was ‘Study whenever you want’, 77 (43.8%), ' Autonomy in time utilization', 53 (30.1%), and ' Speed adjustable', 34 (19.3%). There was no statistically significant difference between male and female, and pre-medical and medical students (p > 0.05) (Table 2).
2) The worst part
The worst part about the online learning environment was ‘Anxiety about learning alone’, 44 (25.0%), and ‘Non-interactive classes’, 30 (17.0%). Analysis of the differences between male and female could not confirm statistically significant differences (p > 0.05) (Table 2).
Among pre-medical students, 16 (21.9%) expressed ‘Anxiety about learning’, 13 (17.8%) ‘Non-interactive classes’, and 13 (17.8%) ‘Disturbance due to location’. Medicine students were analyzed as ‘Anxiety about learning alone’, 28 (27.2%), ‘Disturbance due to location’, 18 (17.5%), and 'Non-interactive classes' 17 (16.5%), and a statistically significant difference was confirmed (p < 0.05) (Table 2).
3) Main place to take classes
The main place to attend classes in the online environment was ‘Home’ for 144 (81.8%), ‘Reading room’ for 16 (9.1%), ‘School’ for 3, and ‘Cafe’ for 8 (4.5%). There was no statistically significant difference between male and female students (p > 0.05) (Table 2).
A statistically significant difference was confirmed between pre-medical and medical students (p < 0.05) (Table 2). The pre-medical students were analyzed in the following order: ‘Home’ 64 (87.7%), ‘School’ 3 (4.1%), ‘Cafe’ 3 (4.1%), and ‘Other’ 3 (4.1%). Medical students were analyzed in the following order: ‘Home’ 80 (77.7%), ‘Reading room’ 13 (12.6%), and ‘Cafe’ 5 (4.9%).
4) What is most needed in an online learning environment
The most necessary things in an online learning environment were ‘Computers such as PCs and laptops’ for 114 (68.4%), ‘Internet, Wi-Fi connections’ for 34 (19.3%), and ‘Space to study’ for 25 (14.2%). There were no statistically significant differences between female and male students and between pre-medical and medical departments (p > 0.05) (Table 2).
3. Differences in living conditions in the COVID-19 pandemic
1) The most difficult thing about school life
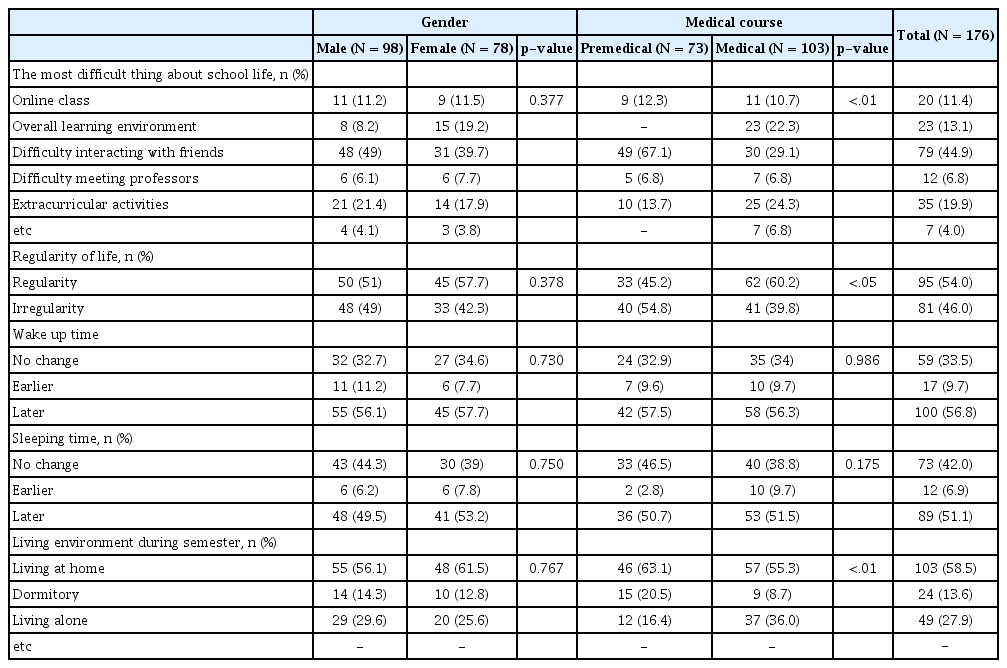
The most difficult aspect of living during the COVID-19 pandemic was 'Difficulty interacting with friends', 79 (44.9%), ‘Extracurricular activities’, 35 (19.9%), and 'Overall learning environment (internet connection, learning location, media preparation for class, etc.)', 23 (13.1%). There was no statistically significant difference between male and female students (p > 0.05) (Table 3).
A statistically significant difference was confirmed between pre-medical and medical students (p < 0.01) (Table 3). Among pre-medical students, 49 (67.1%) had ‘Difficulty interacting with friends’, 10 (13.7%) had ‘Extracurricular activities’ and 9 (12.3%) had ‘Online class’. For medical students, 30 (39.1%) had ‘Difficulty interacting with friends’, 25 (24.3%) had, ‘Extracurricular activities’ and 11 (10.7%) had ‘Online class’.
2) Regularity of life
Regarding regularity of life, 95 (54.0%) responded that they lead ‘Irregularity’, and 81 (46%) responded that they lead an irregular life, and there was no statistically significant difference between male and female students (p > 0.05) (Table 3). A statistically significant difference was found between pre-medical and medical students (p < 0.05) (Table 3). It was analyzed that 33 (45.2%) of pre-medical students and 62 (60.2%) of medical students led ‘Regularity’.
3) Wake up time and sleeping time
It was analyzed that students in the COVID-19 pandemic situation wake up later and go to bed later than before. The waking up time was ‘Later’ for 100 (56.8%), ‘No change’ for 59 (33.5%), and ‘Earlier’ for 17 (9.7%). The sleeping time was ‘Later’ for 89 (51.1%), ‘No change’ for 73 (42.0%), and ‘Earlier’ for 12 (6.9%). There was no statistically significant difference between male and female students in both waking up time and going to bed, and there was no statistically significant difference between premedical and medical students (p < 0.05) (Table 3).
4) Living environment during semester
The residential environment of students during the semester amid the COVID-19 pandemic was analyzed as follows: 103 (58.5%) ‘Living at home’, 49 (27.9%) ‘Living alone’, and 24 (13.6%) ‘Dormitory’. There was no statistically significant difference between female and male students (p > 0.05) (Table 3). There was a statistically significant difference between pre-medical and medical students (p < 0.01) (Table 3). The pre-medical students were analyzed as follows: 46 (63.1%) ‘Living at home’, 15 (20.5%) ‘Dormitory’, and 12 (16.4%) ‘Living alone’. Among the medical students, 57 (55.3%) ‘Living at home’, 37 (36.0%) ‘Living alone’, and 9 (8.7%) ‘Dormitory’.
4. Differences in sleep time in the COVID-19 pandemic
In the COVID-19 pandemic, the average sleep time of medical students is 7.3 hours. Although there was no statistically significant difference between male and female students (p > 0.05) (Table 3), the average sleep time of pre-medical students was 7.75, and the average sleep time of medical students was 7.03, confirming a statistically significant difference (p < 0.01) (Table 4).
Discussion
This study investigated the online learning environment and the overall learning environment of medical students in Daegu and Gyeongbuk, which were selected as the first special disaster area in Korea due to the rapid spread of the COVID-19 pandemic. As a result of the study, differences by gender did not appear in all items, and it was confirmed that there were differences between pre-medical and medical students in the online learning environment and life amid the COVID-19 pandemic. Based on the above analysis results, the following suggestions can be made.
First, it was found that the learning environment, where most classes are conducted online, allows students to study at their own time and allows free use of time, which is better than before the COVID-19 pandemic for medical students. And this is related to the characteristics of medical school education. Compared to most other colleges, medical schools have longer study periods, more credits to complete, and more frequent exams, so students have a high level of pressure about exams and anxiety about repeating grades and grades. In addition, since a large amount of learning is required of medical students to complete and follow the medical school curriculum, it has been reported for a long time that students have a relative lack of time and suffer from insufficient rest time and sleep deprivation [16,17]. Concerns regarding mental health issues, including severe burnout, have been reported among medical students due to the tight curriculum and academic demands of medical schools. As solutions related to this, the need for sufficient rest time and the importance of well-being among medical students have been reported [18-21]. Due to the COVID-19 pandemic, medical school education unintentionally became an online-centered learning, and it was found that securing time autonomy could provide medical students with time for rest and well-being. In the post-corona era, medical schools need to review online learning differently than before based on past experiences, and continuous interest and efforts are needed to support and expand the online learning environment when necessary.
Second, it was analyzed that the biggest difficulty faced by medical students in the online learning environment is that, unlike before, they feel anxious because they are learning alone without going to school and are not sure if they are doing it properly. It was analyzed that pre-medical students had great difficulty with the lack of interaction in class, and medical students had great difficulty with being interrupted in class by the place called home.
In addition, amid the COVID-19 pandemic, the place where most medical students participated in classes was at home. However, it was analyzed that most pre-medical students participated in classes at home and school, and that most medical students participated in classes at home and in the reading room, which showed the difference between pre-medical and medical students. These results show that medical students place more emphasis on a concentrating study environment and academic achievement than premedical students. Similar to these results, it has been reported that it is related to the learning context of medical students according to Korea's medical education curriculum. Medical students learn in earnest the knowledge of basic medicine and clinical medicine necessary for future doctors [22], and as the number of credits earned and the amount of learning increases, it can be seen that places that interfere with concentration are factors that cause many difficulties in learning. A previous study also reported that medical students had greater academic and exam burden and related burnout than premedical students [23]. Therefore, medical schools should consider providing physical support for medical students' learning.
Third, in the COVID-19 pandemic differences in various aspects of the lives of pre-medical and medical students were confirmed. In the COVID-19 pandemic situation, medical students led a more regular life than pre-medical students, and the average sleep time was 7.3 hours, while pre-medical students slept 7.8 hours and medical students 7.03 hours, showing the difference between pre-medical and medical students. These results show that sleep time has increased compared to medical students before the COVID-19 pandemic. Previous studies have shown that medical students lack sleep time due to heavy exams and study load [24], and the sleep time of Korean medical students has been reported to range from as little as 5.5 hours to as much as 6.5 hours in previous studies [25-27]. However, due to the COVID-19 pandemic, it was confirmed that the sleep time of medical students increased due to non-face-to-face classes [22], and this study also found that the average sleep time increased compared to before.
Due to the sudden COVID-19 pandemic, we were unintentionally faced with an online learning environment that we could not choose according to national policy. Medical students took care of the physical resources previously provided for classes and medical school studies on their own, and were able to see the need for these physical resources. In the post-corona era, we will continue to pay attention to a better educational environment for medical students based on this, and we will need to prepare for sudden disasters such as infectious disease outbreaks that may occur again.
Limitations of this study include that it targeted a specific university and that the response rate was low due to the tightness of the medical school curriculum. In future research, we propose a study targeting a broader group to complement these limitations.
Notes
Conflict of interest
The authors declare no conflicts-of-interest related to this article.